This is the second in a two part series on shoulder labral tears. To learn more about the anatomy and function of the shoulder labrum reviewed in the first part, please see my previous post- Shoulder Labral Tear- Relevant Anatomy and Function. With a labral tear, the stability of the shoulder is affected. Along with the labrum, the ligaments and muscles around the shoulder confer stability to the joint. Micro-instability of the shoulder manifests itself as pain and discomfort in certain provocative positions that stress the affected portion of the labrum. Treatments for a labral tear can range from observation and activity modification to surgical labral repair. Read on below to learn more
Nonoperative Treatment
The labrum is like a rubber band that helps hold the humeral head centered on the shoulder socket or glenoid. Depending on the position of the shoulder in space, certain parts of the labrum experience more stress than others. Therefore, engaging in any activity that places pressure or stress on the injured part of the labrum will generate symptoms. Upon recognition of a labral injury, if it is acute, the first step is controlling the associated pain and inflammation. Some physicians may recommend a short period of immobilization in a sling for 1-2 weeks while the swelling subsides. To address the acute inflammation, over the counter anti-inflammatories or prescription strength anti-inflammatories in conjunction with periodic ice pack applications can be used. Once the pain and swelling have decreased, the focus shifts to restoring range of motion. At this point contact sports and strenuous activities are to be avoided.
 Shoulder stabilizing brace attached to right shoulder that restricts shoulder motion
Shoulder stabilizing brace attached to right shoulder that restricts shoulder motionThe next step in treatment is largely dictated by the patients goals and objectives. Whether or not to proceed directly to surgery to repair an injured labrum is controversial depending on the portion of the labrum affected. My approach is tailored to the individuals expectations and requirements. For patients with a sedentary lifestyle and a stable shoulder, sometimes avoiding the vulnerable or painful provocative shoulder positions is the simplest of solutions once the acute pain and inflammation resolve.
For patients that place more demands on their shoulder because of sports or occupation, observation alone is not a viable strategy. In these circumstances, I first recommend a course of formal shoulder rehabilitation focused on developing rotator cuff muscle strength and coordination. Depending on the extent of the labral injury, and if there is any associated bone injury as well, increased strength of the rotator cuff muscles can often stabilize the shoulder sufficiently to overcome the loss of stability from an injured labrum. Once full motion and strength of the shoulder is restored, I permit a return to sports. In some situations a brace may be used to limit the extremes of shoulder range of motion when playing contact sports. The brace (pictured on the right) may not work for all athletes. A lineman for example may find it more suitable than a wide receiver that needs to elevate his arm. If in spite of aggressive shoulder rehabilitation the injured labrum remains symptomatic and/or the shoulder dislocates, then shoulder surgery to address the damaged labrum is recommended.
Operative Treatment
 Anterior dislocation of the shoulder is one mechanism of labrum injury
Anterior dislocation of the shoulder is one mechanism of labrum injuryThere is growing evidence in the athlete population that proceeding directly to surgery after a shoulder dislocation to repair the labrum damage is better than a trial of physical therapy and competitive play. Given the evolving nature of this evidence, I generally recommend at least one trial of physical therapy before proceeding to surgery. If after returning to play the athlete sustains another dislocation, then I recommend no further participation until the labral damage is repaired. Successive dislocations have been shown to damage the joint and increase the rate of shoulder arthritis in the future. For the appropriate candidate, surgery can restore the shoulder stability and permit a return to sport.
Labral repair of the shoulder can be performed arthroscopically in a minimally invasive way. Historically the surgery was performed using an incision overlying the shoulder. As modern techniques have evolved, the outcomes from arthroscopic labral repair are now comparable, if not better, than open shoulder surgery. The surgery is performed as an outpatient surgery and generally takes 1-2 hours to do.
Pre-operative Preparation
After midnight before surgery, all food and drink must be discontinued. This is to ensure your stomach is empty for anesthesia and surgery. On the day of surgery the anesthesiologist will administer medications around your neck area to perform a “nerve block”. This technique temporarily numbs the nerves of the entire arm for surgery and reduces the amount of anesthetic drugs needed to keep you comfortable. Once you are asleep, you are positioned on your side for the duration of the surgery with your injured shoulder facing up. Care is taken to ensure you are positioned comfortably and that there are no pressure points. Antibiotics are given intravenously to reduce the risk of infection. The skin is sterilized using aseptic cleaning agents. The arm is suspended using a crane like device and distracted using
Labral Repair Operation
The camera is inserted next through a small 1 cm incision on the posterior part of the shoulder. Additional access points are established from the front part of the shoulder to insert instruments and probes. A systematic inspection of the entire joint is performed next to evaluate the extent of labral damage.
The first slide in the slideshow below illustrates the camera (black tube) and the associated camera view (blue rectangle) of the shoulder (humeral head seen in top of camera image) resting in its socket, the glenoid (seen in bottom of camera image), and the labral tear. The head of the patient would be to the left of the image shown. An anterior dislocation of the shoulder is the most common cause of labral injury and is the mechanism for the injury shown here.
After the inspection is complete, the labral tear is probed and explored. If it has been some time since the injury, often the labrum is scarred below the rim of the glenoid and must be liberated of any restraining scar tissue using specialized instruments before repair. Once the labrum has been mobilized, dis-solvable anchors are implanted along the rim of the glenoid.
These anchors look like sheet-rock screws with sutures attached to the top. After implanting the anchors, the free sutures are passed around the torn labrum.
Next the sutures are secured with knots around the torn labrum, bringing the labrum back to its anatomical position. Enough anchors to secure the labrum back to glenoid are used. Newer anchor implants now incorporate mechanisms that secure the sutures around the labrum without any bulky knots.





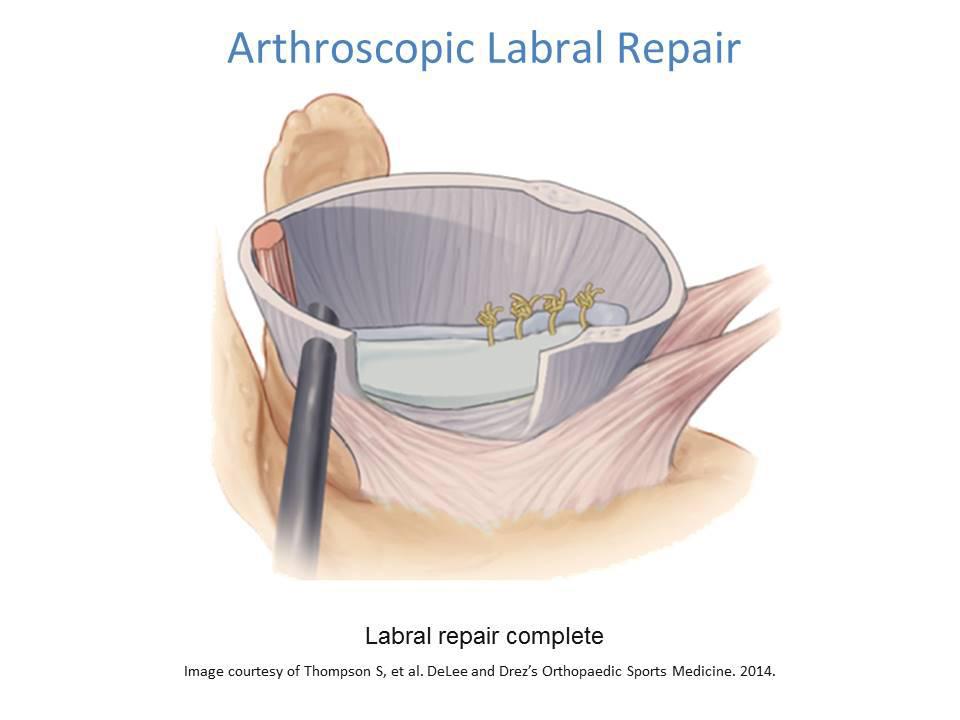
Upon completion of the labral repair, the labrum’s function as a bumper around the lip of the glenoid has been restored.
Often in addition to the labral tear there is concomitant stretching of the capsule that surrounds the shoulder from the time of injury. Tightening of the capsule can be performed at the time of labral repair too by stitching the loose redundant capsular tissue.
Post-operative Recovery
After labral repair, for the first 4-6 weeks a shoulder immobilizing brace is used to prevent shoulder movement and protect the repair. Immobilization of any joint for so long results in scar tissue and loss of motion. Once the repair has had an opportunity to heal, the first phase of rehabilitation involves restoration of joint motion. With the help of a physical therapist, the shoulder is stretched to gradually work through the scar tissue that naturally develops after a period of joint immobilization.
Once the full range of motion has been obtained, the focus shifts to muscle strengthening. This includes not only the rotator cuff muscles, but also the muscles surrounding the shoulder blade and the muscles that maintain your posture. Once adequate strength has been restored, sports specific drills are incorporated for neuromuscular training and preparation. Based on your progression through therapy, clearance for sports participation can be expected typically 4-6 months after the surgery.
Read the first part of this series in my post- Shoulder Labral Tear- Relevant Anatomy and Function, to learn more about the labral anatomy. Or explore the other arthroscopic shoulder surgeries I perform. Call 281-690-4678 now to schedule a consultation to discuss your labral injury or labral repair.
Sources:
http://orthoinfo.aaos.org/topic.cfm?topic=a00426https://www.ncbi.nlm.nih.gov/pubmed/6476187https://www.ncbi.nlm.nih.gov/pubmed/19254851https://www.ncbi.nlm.nih.gov/pubmed/8934481